BLOG
Fat loss injections. Can they really silence "Food Noise?"
Written by Jennifer Thawley, BSc (Hons), PG Dip, RD, April, 2025

There’s a real hype around fat loss injections at the minute. You may also know them as GLP-1 medications that go by the names of Semaglutide (Ozempic, Weygovy) or Liraglutide (Saxenda).
There are many people sitting on endless waiting lists to get them from their NHS doctor and many are paying hundreds of pounds to buy them online for their ability to help people achieve impressive weight loss results.
As a specialist dietitian I’ve been supporting people using GLP-1s for weight management in type 2 diabetes for many years and I often hear clients say;
“I no longer think about food all the time, it’s silenced the food noise.”
But what does this actually mean—and is it not simply all just down to side effects?
Let’s look at what’s happening in the body and brain—and how food and lifestyle still play a key role in the journey.
What Is “Food Noise?”
“Food noise” is a term people often use to describe constant, intrusive thoughts about food—from cravings and snacking habits to emotional triggers and compulsive eating. If you’ve struggled with overeating, bingeing, or food preoccupation, you’re not alone. GLP-1 medications have been found to significantly reduce these cravings. But why?
It's in the way GLP-1s work
GLP-1 (Glucagon-Like Peptide-1) is a natural hormone that helps us to feel full. GLP-1 medications mimic this hormone and work in multiple ways:
- In the Stomach: They slow stomach emptying, helping you feel fuller for longer. This also causes many side effects from bloating, reflux, nausea, vomiting, diarrhoea and constipation. This inevitably results in a person eating far less than they did before which results in significant weight loss.
- In the Brain: They target appetite control centres in the brain. This affects our reward pathways which help to reduce cravings and the emotional drive to eat. Many users report that the reduced food preoccupation continues even after those side effects fade. That’s because the brain effect is distinct and longer-lasting.
- In the Pancreas and Liver: They help the pancreas to release insulin when it is needed and stops the liver for making extra glucose when it isn't and this is why these medications are particularly good for helping people with Type 2 Diabetes to manage their blood glucose levels.
Studies on the brain show that GLP-1 medications reduce brain activity in regions linked to food reward and motivation—which helps explain why many people feel more in control and less “mentally hungry.”
But there's some concerns around GLP-1 medications;
Side effects such as nausea, vomiting and diarrhoea can vary from mild to quite severe. Concerns I often have when people suffer significantly with these symptoms is that they are simply not getting a safe level of nutrients or fluid. I find many who take them don't want to tell anyone that they are having such terrible side effects through fear of it being stopped. Those with severe side effects are at increased risk of dehydration and kidney failure if they do not drink enough fluid daily.
It almost puts a new meaning into "dying to be thin!"
Other recognised concerns include;
- Risk of inflamed pancreas, also known as acute pancreatitis.
- Women taking oral contraceptive medications are at risk of becoming pregnant as vomiting and diarrhoea reduces their effectiveness.
- Women taking HRT may also find their treatment is not as effective.
- More recently studies have been raising concerns around the effects of bone and muscle loss as a result of such drastic weight loss in such a short space of time. This is a particular concern for women entering the perimenopause and menopause as they are already losing muscle and bone mass at an increased rate due to the loss of oestrogen.
Why you need a Dietitian
In the real world most individuals take GLP-1 fat loss injections with no input from a nutritionist or dietitian despite the research showing that the incredible weight loss seen in the studies was a result of all participants being given diet, lifestyle and behaviour change support.
Even with the help of GLP-1 medication, your long-term success depends on sustainable dietary habits, behaviour change, and lifestyle support. That’s where working with a registered dietitian can make all the difference.
How I Can Help
As a UK-registered dietitian, I offer personalised support for:
- Meal planning on GLP-1s (what to eat when your appetite is low)
- Managing nausea and side effects through diet
- Balancing protein, fibre, and fats to support blood sugar and satiety
- Avoiding under-nutrition and muscle loss during weight loss
- Rebuilding a healthy relationship with food, free from guilt or obsession
Whether you’re new to GLP-1 therapy or adjusting to a changed appetite, you deserve tailored, evidence-based support—not a one-size-fits-all diet plan.
Let’s Work Together
Contact me to learn more about 1:1 nutrition support for GLP-1 users.
How To Manage Menopause Symptoms Naturally: What Really Works (and what doesn’t!)
Find out which evidence based diet and lifestyle changes truly help with weight gain and symptoms of perimenopause and menopause. Skip the fads- discover the real game changers.
Written by Jennifer Thawley, BSc (Hons), PG Dip, RD, May, 2025

Menopause is a natural phase of life, but the physical and emotional symptoms can feel anything but normal.
80% of women will suffer from a symptom of Peri/menopause with 25% suffering from debilitating symptoms.
Given that 50% of the population will very likely begin this journey from peri to menopausal between the ages of 41 to 55 , it’s fair to say that this isn’t just a ‘girl problem’. This can affect families, and work places significantly.
1 in 10 women leave their jobs due to unmanaged symptoms.
The UK’s National Institute for Health and Care Excellence (NICE) updated it’s menopause guideline back in November 2024 (Information for the public | Menopause: identification and management | Guidance | NICE) and since then there’s been a real spotlight on the significant effects perimenopause and menopause can have on a woman, both physically and emotionally.
What’s great is that this issue has been further pushed to the forefront of health agendas after Davina McCall opened up so candidly about it. She originally made the Channel 4 documentary Sex, Myths and the Menopause and has been on a mission to open up the conversation about it ever since.
(Watch Davina McCall: Sex, Myths and the Menopause | Stream free on Channel 4)
I enjoyed listening to Davina talk about the subject on the Zoe Podcast- Davina McCall: Make these daily choices and live your life you deserve on Spotify and You Tube. Davina herself really promotes the benefits of a healthy diet for menopause and how it can offer more natural menopause symptom relief.
Many refer to this movement as the ‘Davina effect’ and I’m all for it!
With better knowledge and understanding of peri/menopause women are more likely to access the correct medical treatment and feel more empowered to make the right lifestyle choices to thrive rather than simply survive!
Although, I feel there’s also huge downside to this as the health industry is now booming with supplements, diets, exercise plans, shampoos and creams all promising to cure symptoms peri/menopause.
Women are led to believe there’s a complex formula for success. When the reality is that most of these “special menopause” products have very little quality evidence behind them and as women hyperfocus on these they neglect the REAL game changers!
As specialist dietitian here’s the top 6 things I advise for success!
1. Prioritise Protein intake
After the age of 35 our muscle mass naturally starts to decline, and this process accelerates during peri/menopause due to falling Oestrogen levels. Adequate protein intake supports muscle maintenance and helps us to maintain a higher calorie requirement which in turn can help prevent weight gain.
What can I do?
- Aim for 1.2–1.5 grams of protein per kilogram of ideal body weight daily. Include a portion of protein-rich foods like eggs, fish, poultry, tofu, beans/lentils, Greek yoghurt, milk or cottage cheese in each meal.
2. Support your bone health with Calcium and Vitamin D
Postmenopausal women are at increased risk of osteoporosis due to declining oestrogen levels. In fact 1 in 3 women have Osteoporosis and 50% will suffer a bone fracture as a result.
What can I do?
- Aim to have at least 3 portions of food high in calcium each day through dairy products such as milk, yoghurt, cheese (including fortified alternatives), and leafy greens.
Check out your intake of calcium with the international osteoporosis foundation Calcium calculator: CALCIUM - Calcium Calculator | International Osteoporosis Foundation
Vitamin D
Is also essential for calcium absorption and is the only supplement recommended by the British Menopause Society. Around 25% of the population don’t get enough vitamin D. Our main source is sunlight, which helps our skin produce an active form of the vitamin. However, as we age—especially over 65—our skin becomes less efficient at making it. People with darker skin tones (African Caribbean or South Asian origin) also produce less vitamin D.
Low vitamin D levels can lead to fatigue, weakness, muscle, back, or bone pain, increased infections, slower wound healing, low mood, and even depression. Long-term deficiency may raise the risk of type 2 diabetes, heart disease, weight gain, and some cancers.
Dietary sources include oily fish (like salmon, mackerel, and sardines), egg yolks, red meat, and liver. Some foods are fortified with vitamin D, such as cereals, plant milks, and spreads. Still, food alone usually doesn’t provide enough.
What can I do?
Take a 10 microgram Vitamin D3 supplement daily between the months of September to April. However this amount would also be safe to take all year round!
3. Extreme Diets don’t work
Although there are a whole host of diets recommended for menopause (Keto, Carnivore, Intermittent Fasting, Low Carb, Vegan… the list goes on!) the truth is none of these diets have solid evidence to prove their superiority over each other for weight loss or symptom management.
I often talk to my clients about what foods they enjoy most and we then look at how we can come up with a plan that ensure they are consistent with diet over the long term. It is this that helps them to reach their goals!
Choosing overly restrictive diets, and diets that cut whole food groups out simply aren’t achievable and increase the risk of nutritional deficiency. Above all very restrictive diets (<1200Kcal per day) can also promote muscle and bone loss!
Furthermore most women I meet are already suffering with symptoms such as poor sleep, IBS symptoms, fatigue and low mood. Attempting some wild diet really isn’t going to help the situation!
It’s about focussing on getting all the nutrients your body needs to fuel weight loss through peri/menopause.
4. Focus on fibre for gut health
During Peri/menopause many women can start to intermittently have digestive issues such as bloating, wind, indigestion, constipation and diarrhoea.
This is because rising and falling levels of Oestrogen and Progesterone affect our gut motility. This results in an imbalance in healthy gut bacteria leading to inflammation.
Fibre rich foods don’t just help move things along in the bathroom department. They’re also rich sources of Prebiotics which support our healthy gut bacteria to protect us from inflammation.
What can I do?
- Eating a wide variety of fruits and vegetables of all types and colours can significantly increase the amount and diversity of our gut bacteria. Specifically beneficial foods include garlic, broccoli, cabbage, leeks, bananas, and apples.
But what about probiotics?
Probiotics are very exiting area of research and there are many studies showing the varied benefits of Probiotics for gut health however not so much directly in relation to Menopause.
There’s a vast choice of products from probiotic yoghurts, drinks, capsules, and powders however in order to get the beneficial effects it is important for Probiotics to be able to arrive, survive and thrive in great numbers by the time the reach the gut. However probiotics aren’t highly regulated and not all are of good quality.
What can I do?
If you'd like to try a probiotic both Symprove Probiotic Supplement - 20% Discount Code and Actimel - The cultured yogurt shot that's got a lot | Actimel are good quality probiotics and have been shown to reduce digestive issues including IBS symptoms. But watch this space for more exiting research in to menopause specific benefits!
It's important to take any probiotic as directed for at least 3 months to see the benefits.
5. Raise your heart rate and lift some weights
Menopause increases a woman’s risk of heart disease, diabetes and osteoporosis. Physical activity in the form of exercise which raises your heart rate and exercises which involve lifting weights is essential not only to promote heart health, it improves insulin sensitivity and supports bone strength. Aside from these 3 things it can help maintain your calorie output supporting weight loss.
What can I do?
- Move 4-5 days of the week and sit less
- Aim to do 2 hrs and 30 minutes of moderate cardio, or 1 hour 15 minutes of vigorous Cardio per week- this might include power waling, swimming, aerobics, cycling, dancing or jogging
- Strength training 2 days a week- lifting some weights, doing body weight exercises or using resistance bands
- Consider getting a fitness tracker to help motivate you!
The NHS website has some really great pointers on how you can increase your activity, including videos Exercise - NHS
6. Manage stress and prioritise sleep
Chronic stress and poor sleep can exacerbate menopausal symptoms and hinder weight management.
Managing stress is easier said than done when you have a family to care for, a job to hold down and just the daily stressors of life but it really is so important to look for small snippets of time in your day or week to incorporate stress-reduction techniques such as mindfulness, yoga, or meditation.
What Can I do?
- Download a mindfulness app. For example- Headspace offer short 5-10 minute meditation sessions. Headspace Content | Meditation & Sleep App
- Aim for 7–9 hours of quality sleep per night. Think about avoiding blue light from phone and tablet screens in the hours running up to bed. Maybe use the last half an hour of your day to focus on meditation or some breathing exercises before you sleep.
Bottom line….
You can get all the nutrients you require from a varied diet. Stop wasting your hard earned money on pills and potions.
You really don’t need to be depriving yourself of the foods you love, nor do you need to be focussing on eating specific foods at specific times.
Menopause is an opportunity for you to break free from yo-yo dieting and choose a plan that you can make into a lifestyle rather than a quick fix.
Let's work together
If you’re struggling to navigate through weight changes or symptoms during perimenopause/menopause I can help. Book a 1 to 1 consultation today and take the first step towards feeling in control again.
The Power of Protein for Weight Loss
Protein isn’t just for body builders! Find out how protein boosts fullness, supports weight loss and why it is essential for maintaining muscle and bone strength.
Written by Jennifer Thawley, BSc (Hons), PG Dip, RD, May, 2025

Menopause is a natural phase of life, but the physical and emotional symptoms can feel anything but normal.
80% of women will suffer from a symptom of Peri/menopause with 25% suffering from debilitating symptoms.
Given that 50% of the population will very likely begin this journey from peri to menopausal between the ages of 41 to 55 , it’s fair to say that this isn’t just a ‘girl problem’. This can affect families, and work places significantly.
1 in 10 women leave their jobs due to unmanaged symptoms.
The UK’s National Institute for Health and Care Excellence (NICE) updated it’s menopause guideline back in November 2024 (Information for the public | Menopause: identification and management | Guidance | NICE) and since then there’s been a real spotlight on the significant effects perimenopause and menopause can have on a woman, both physically and emotionally.
What’s great is that this issue has been further pushed to the forefront of health agendas after Davina McCall opened up so candidly about it. She originally made the Channel 4 documentary Sex, Myths and the Menopause and has been on a mission to open up the conversation about it ever since.
(Watch Davina McCall: Sex, Myths and the Menopause | Stream free on Channel 4)
I enjoyed listening to Davina talk about the subject on the Zoe Podcast- Davina McCall: Make these daily choices and live your life you deserve on Spotify and You Tube. Davina herself really promotes the benefits of a healthy diet for menopause and how it can offer more natural menopause symptom relief.
Many refer to this movement as the ‘Davina effect’ and I’m all for it!
With better knowledge and understanding of peri/menopause women are more likely to access the correct medical treatment and feel more empowered to make the right lifestyle choices to thrive rather than simply survive!
Although, I feel there’s also huge downside to this as the health industry is now booming with supplements, diets, exercise plans, shampoos and creams all promising to cure symptoms peri/menopause.
Women are led to believe there’s a complex formula for success. When the reality is that most of these “special menopause” products have very little quality evidence behind them and as women hyperfocus on these they neglect the REAL game changers!
As specialist dietitian here’s the top 6 things I advise for success!
1. Prioritise Protein intake
After the age of 35 our muscle mass naturally starts to decline, and this process accelerates during peri/menopause due to falling Oestrogen levels. Adequate protein intake supports muscle maintenance and helps us to maintain a higher calorie requirement which in turn can help prevent weight gain.
What can I do?
- Aim for 1.2–1.5 grams of protein per kilogram of ideal body weight daily. Include a portion of protein-rich foods like eggs, fish, poultry, tofu, beans/lentils, Greek yoghurt, milk or cottage cheese in each meal.
2. Support your bone health with Calcium and Vitamin D
Postmenopausal women are at increased risk of osteoporosis due to declining oestrogen levels. In fact 1 in 3 women have Osteoporosis and 50% will suffer a bone fracture as a result.
What can I do?
- Aim to have at least 3 portions of food high in calcium each day through dairy products such as milk, yoghurt, cheese (including fortified alternatives), and leafy greens.
Check out your intake of calcium with the international osteoporosis foundation Calcium calculator: CALCIUM - Calcium Calculator | International Osteoporosis Foundation
Vitamin D
Is also essential for calcium absorption and is the only supplement recommended by the British Menopause Society. Around 25% of the population don’t get enough vitamin D. Our main source is sunlight, which helps our skin produce an active form of the vitamin. However, as we age—especially over 65—our skin becomes less efficient at making it. People with darker skin tones (African Caribbean or South Asian origin) also produce less vitamin D.
Low vitamin D levels can lead to fatigue, weakness, muscle, back, or bone pain, increased infections, slower wound healing, low mood, and even depression. Long-term deficiency may raise the risk of type 2 diabetes, heart disease, weight gain, and some cancers.
Dietary sources include oily fish (like salmon, mackerel, and sardines), egg yolks, red meat, and liver. Some foods are fortified with vitamin D, such as cereals, plant milks, and spreads. Still, food alone usually doesn’t provide enough.
What can I do?
Take a 10 microgram Vitamin D3 supplement daily between the months of September to April. However this amount would also be safe to take all year round!
3. Extreme Diets don’t work
Although there are a whole host of diets recommended for menopause (Keto, Carnivore, Intermittent Fasting, Low Carb, Vegan… the list goes on!) the truth is none of these diets have solid evidence to prove their superiority over each other for weight loss or symptom management.
I often talk to my clients about what foods they enjoy most and we then look at how we can come up with a plan that ensure they are consistent with diet over the long term. It is this that helps them to reach their goals!
Choosing overly restrictive diets, and diets that cut whole food groups out simply aren’t achievable and increase the risk of nutritional deficiency. Above all very restrictive diets (<1200Kcal per day) can also promote muscle and bone loss!
Furthermore most women I meet are already suffering with symptoms such as poor sleep, IBS symptoms, fatigue and low mood. Attempting some wild diet really isn’t going to help the situation!
It’s about focussing on getting all the nutrients your body needs to fuel weight loss through peri/menopause.
4. Focus on fibre for gut health
During Peri/menopause many women can start to intermittently have digestive issues such as bloating, wind, indigestion, constipation and diarrhoea.
This is because rising and falling levels of Oestrogen and Progesterone affect our gut motility. This results in an imbalance in healthy gut bacteria leading to inflammation.
Fibre rich foods don’t just help move things along in the bathroom department. They’re also rich sources of Prebiotics which support our healthy gut bacteria to protect us from inflammation.
What can I do?
- Eating a wide variety of fruits and vegetables of all types and colours can significantly increase the amount and diversity of our gut bacteria. Specifically beneficial foods include garlic, broccoli, cabbage, leeks, bananas, and apples.
But what about probiotics?
Probiotics are very exiting area of research and there are many studies showing the varied benefits of Probiotics for gut health however not so much directly in relation to Menopause.
There’s a vast choice of products from probiotic yoghurts, drinks, capsules, and powders however in order to get the beneficial effects it is important for Probiotics to be able to arrive, survive and thrive in great numbers by the time the reach the gut. However probiotics aren’t highly regulated and not all are of good quality.
What can I do?
If you'd like to try a probiotic both Symprove Probiotic Supplement - 20% Discount Code and Actimel - The cultured yogurt shot that's got a lot | Actimel are good quality probiotics and have been shown to reduce digestive issues including IBS symptoms. But watch this space for more exiting research in to menopause specific benefits!
It's important to take any probiotic as directed for at least 3 months to see the benefits.
5. Raise your heart rate and lift some weights
Menopause increases a woman’s risk of heart disease, diabetes and osteoporosis. Physical activity in the form of exercise which raises your heart rate and exercises which involve lifting weights is essential not only to promote heart health, it improves insulin sensitivity and supports bone strength. Aside from these 3 things it can help maintain your calorie output supporting weight loss.
What can I do?
- Move 4-5 days of the week and sit less
- Aim to do 2 hrs and 30 minutes of moderate cardio, or 1 hour 15 minutes of vigorous Cardio per week- this might include power waling, swimming, aerobics, cycling, dancing or jogging
- Strength training 2 days a week- lifting some weights, doing body weight exercises or using resistance bands
- Consider getting a fitness tracker to help motivate you!
The NHS website has some really great pointers on how you can increase your activity, including videos Exercise - NHS
6. Manage stress and prioritise sleep
Chronic stress and poor sleep can exacerbate menopausal symptoms and hinder weight management.
Managing stress is easier said than done when you have a family to care for, a job to hold down and just the daily stressors of life but it really is so important to look for small snippets of time in your day or week to incorporate stress-reduction techniques such as mindfulness, yoga, or meditation.
What Can I do?
- Download a mindfulness app. For example- Headspace offer short 5-10 minute meditation sessions. Headspace Content | Meditation & Sleep App
- Aim for 7–9 hours of quality sleep per night. Think about avoiding blue light from phone and tablet screens in the hours running up to bed. Maybe use the last half an hour of your day to focus on meditation or some breathing exercises before you sleep.
Bottom line….
You can get all the nutrients you require from a varied diet. Stop wasting your hard earned money on pills and potions.
You really don’t need to be depriving yourself of the foods you love, nor do you need to be focussing on eating specific foods at specific times.
Menopause is an opportunity for you to break free from yo-yo dieting and choose a plan that you can make into a lifestyle rather than a quick fix.
Let's work together
If you’re struggling to navigate through weight changes or symptoms during perimenopause/menopause I can help. Book a 1 to 1 consultation today and take the first step towards feeling in control again.
Fat Loss Injections (GLP-1 Agonists) What Every Woman Needs To Know
Are you considering taking a fat loss injection such as Ozempic, Weygovy or Mounjaro? Maybe you've already started your journey?
On paper these revolutionary drugs have changed the health and weight loss landscape in so many positive ways! HOWEVER there are some risks that could potentially affect your health significantly and irreparably and these aren't being talked about. Find out how to take fat loss injections the right way here!
Written by Jennifer Thawley, BSc (Hons), PG Dip, RD, June, 2025

Perimenopause and Menopause is coming to all women and they bring a host of changes—hormonal shifts, metabolic slow-down, and unfortunately, weight gain.
Over 50% of women can gain an average of 10 kg within a year of menopause.
This is driven largely by the drop in Oestrogen and its ripple effects on sleep, mood, muscle mass and insulin sensitivity. Increased visceral fat, insulin resistance, dyslipidaemia and reduced resting metabolic rate (due to muscle loss) all contribute to make weight management a real challenge.
Weight loss injections are clearly proving to be effective in the battle against stubborn weight gain for women and they're now super easy to get your hands on (If you have the money to finance them!)
So How Effective Are Weight loss injections (GLP-1 Agonists) “On Paper”?
GLP-1 agonists such as Semaglutide (Ozempic, Wegovy) and Liraglutide (Saxenda) have revolutionised obesity management—but only as part of a broader plan.
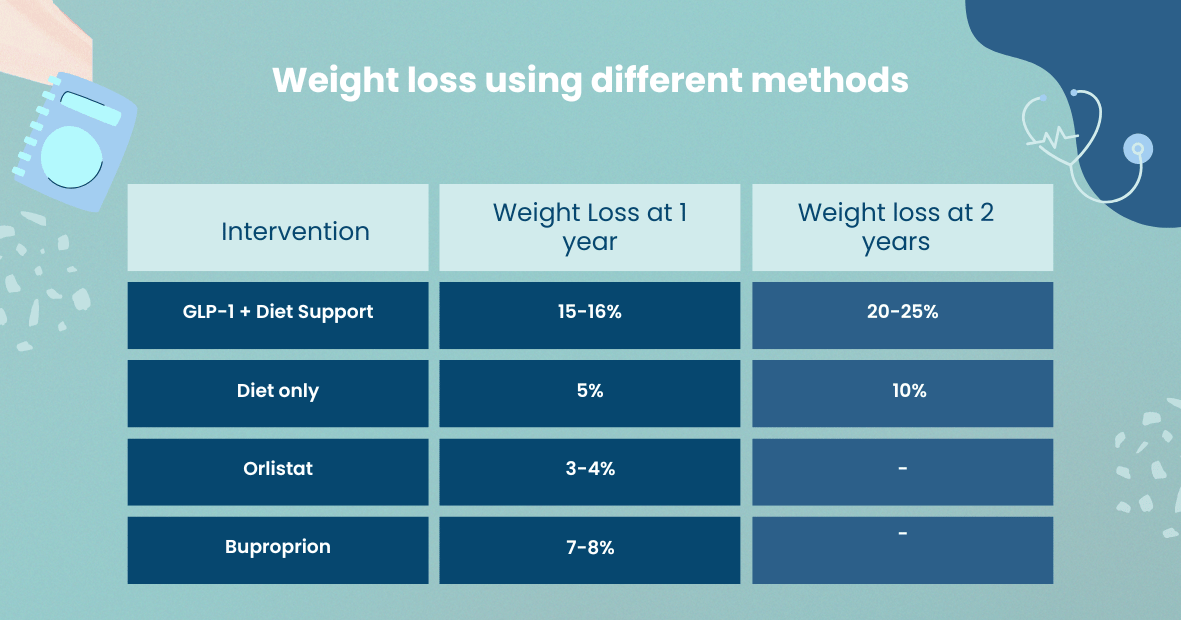
Key point: The table above shows impressive GLP-1 results from the STEP and SCALE trials, where participants received structured diet, exercise and behavioural support to ensure a sustained calorie deficit.
In the real world, that wraparound support is often missing—yet it’s absolutely critical for maximising and maintaining results.
Why Lifestyle & Behaviour Change Matter
Too many women see GLP-1s as a “silver bullet” rather than a powerful tool within a comprehensive weight-management plan. Without:
- Calorie-controlled nutrition
- Regular physical activity
- Sleep optimisation
- Stress management
Weight loss plateaus and regain are all but guaranteed once medication stops (or is reduced).
My approach combines medication oversight with tailored nutrition support to address sugar cravings, low motivation, emotional eating and poor sleep—so you not only lose weight but learn to keep it off for life.
Safety Considerations & Drug Interactions
GLP-1s affect gut transit, which can modify absorption of:
- Oral contraceptives & progestogens: Reduced effectiveness may increase breakthrough bleeding and risk of endometrial complications. Strategies include switching to transdermal HRT or an intrauterine system, or temporarily adjusting progestogen dose.
- Hormone Replacement Therapy: Vomiting or diarrhoea can interfere with HRT absorption. Always disclose GLP-1 use so your HRT regimen can be optimised.
- Other medications: Emerging data (animal and early human studies) raise questions about thyroid safety and renal function—especially if dehydration occurs from GI side effects.
Roughly 10% of users experience nausea, vomiting or diarrhoea.
When rapid weight loss isn’t accompanied by an adequate protein intake and strength training, muscle and bone density can decline—concerns that are amplified in menopausal women already at risk of osteoporosis and sarcopenia. HRT may offer some protective effect, but only if appropriately prescribed and monitored.
How I Can Support You
Lasting change comes from teaming these cutting-edge fat loss injections with personalised lifestyle support. Key considerations that I take in to account when supporting women taking fat loss injections;
- Comprehensive Assessment: Review your medical history, HRT/contraceptive needs and bone health.
- Medication Oversight: Liaise with your GP or specialist to optimise GLP-1 dosing, HRT route and any other prescriptions.
- Nutrition Coaching: Tailored meal plans to ensure protein adequacy, micronutrient balance and a sustainable calorie deficit.
- Symptom Management: Support with eating and drinking when you're feeling nauseous, suffering with vomiting/diarrhoea
- Exercise Programming: Strength training to protect muscle and bone, plus enjoyable cardio to boost sleep and mood.
- Behavioural Tools: Strategies to manage cravings, stress and motivation—so you never feel like you’re on your own.
Ready to take control of your menopausal journey—safely and sustainably?
Contact me today and let’s create your personalised plan for lasting health, vitality and confidence.The
©Copyright. All rights reserved.
We need your consent to load the translations
We use a third-party service to translate the website content that may collect data about your activity. Please review the details in the privacy policy and accept the service to view the translations.